Microscopic diagnosis of acute Malaria – Old but Gold?
The detection under the light microscope has been until now the gold standard for malaria acute diagnosis because it fulfils most of important diagnostic criteria [1]:
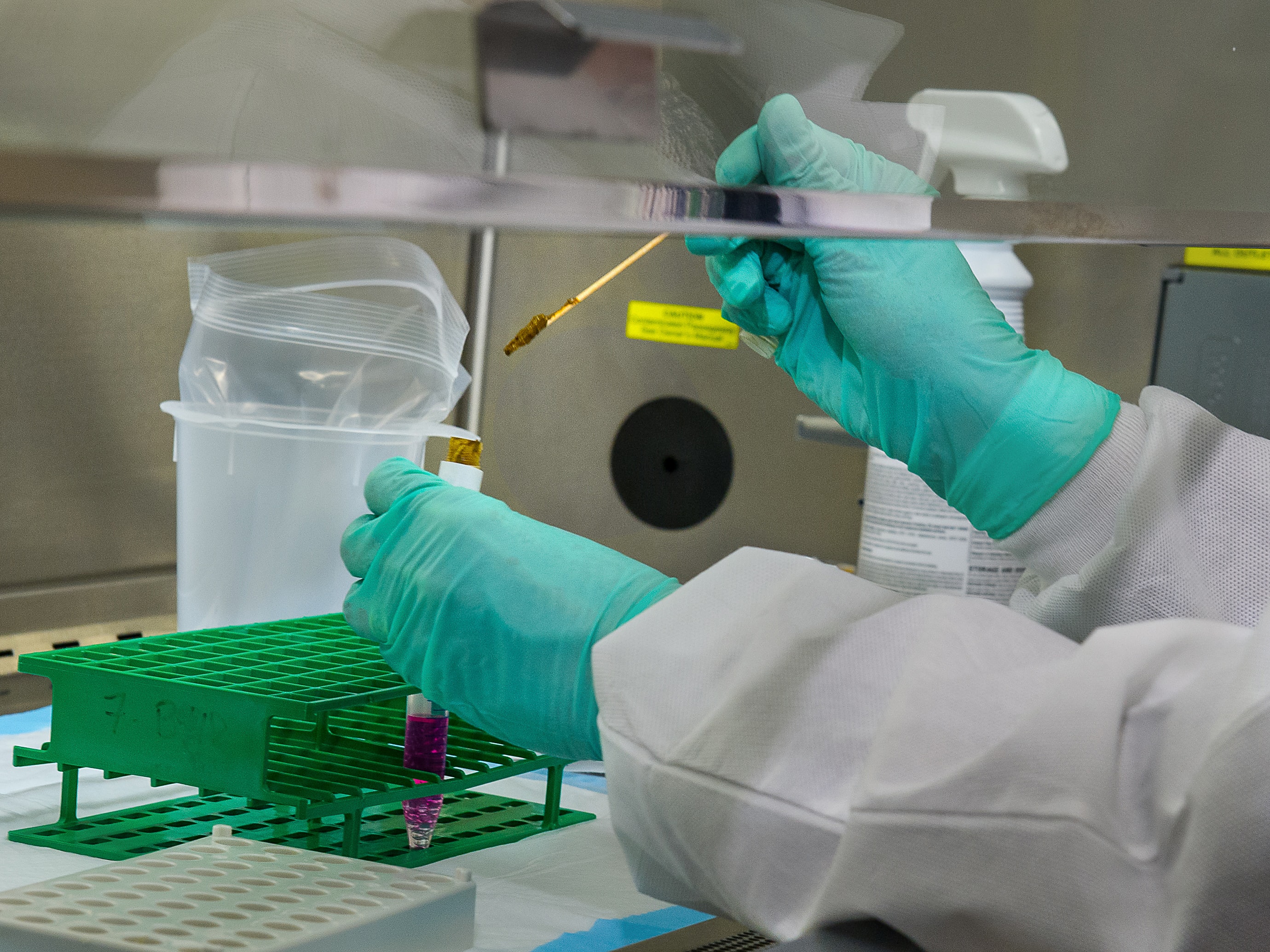
Provided that a trained and skilled lab worker is performing the method and interpretation, Plasmodium parasites can be detected, identified and specified by morphological criteria. Also, differentiation of the life cycle stages of the parasites, quantification, and monitoring the effectiveness of malaria treatment is possible.
The method is easy to perform and relatively low in cost. For microscopic examination, a specimen of the patient’s blood is smeared on microscope slides, one thin layer for quantification and a thick layer for differentiation. After the layers have been stained by giemsa, they are being examinated under the light microscope [1,2].
On the one hand, microscope technique is familiar to most laboratorians in endemic regions, as they are faced with a high frequency of malaria cases and therefore have developed much experience in microscopical diagnosis.
On the other hand, diagnosis by microscopy involves difficulties as it is time consuming and labor-intensive. In spite of being relatively cheap in comparison to other diagnostic methods, light microscopes are not available in all health facilities of less developed areas. Furthermore, quality of results may be affected negatively by high workloads, low level of skill and low stain quality.
Malaria endemic regions are often confronted with other deficits that hinder microscopy service, such as failure of electricity, lack of standard reagents, lack of skilled and trained staff and lack of a good quality assurance program [1,2].
As we can gather from the deficits and from the current situation, there is a need for improvement, and there are considerable reasons why constant progress in diagnostic methods of Malaria should be pursued.
Regarding the useful sides and the disadvantages of different methods, we can summarize the factors an ideal method would include:
An automated method that is easy to perform would be favourable for a high rate sample detection and for lab workers with low level of expertise. Ideally, it should provide rapid and reliable results and be improved by a high sensitivity and high specificity independent from a lab worker’s level of skill. The method should also quantify the number of parasites and not give any false negative or false positive results. Costs should be low. The need for further reagents should be as little as possible and the storage uncomplicated. Lack of electricity should not present a barrier for the method.
Creating the list of ideal criteria is simple. If it is also for the development of the ideal method? Maybe it will take some time, maybe it will not include all qualities. The fact is, there is an urgent need for improvement of methods that apply in both endemic and non-endemic regions. In the attempt to prevent the onset of the disease, death by Malaria and an epidemic spread of the Malaria parasites, a faster, easier and reliable diagnosis is essential.
[1] Labor Diagnostik Karlsruhe
https://www.labor-karlsruhe.de/lv/?module=Analyte&action=einzel&id=1764
[2] Deutsche Gesellschaft für Tropenmedizin
und Globale Gesundheit e.V.
Malariaempfehlungen; Malariaprophylaxe
https://www.dtg.org/empfehlungen-und-leitlinien/empfehlungen/malaria.html
Photo credit: “Sorting mosquitoes” by World Malaria Day is licensed under CC BY-NC-N